AIDET ( acknowledge, identify, duration, explain and thank you)
Subjective Data: PMH, cough ( type; productive, nonproductive, dry, wet) phlegm ( color), nocturnal cough, SOB ( activity or rest). Medication. Smoke ( how much, how long, cessation, second hand, type smoke) and work environment. Sleep pattern and how pt. sleep ( number pillow or recliner etc…) night sweat, weight loss, and medication ( o2 or ace/arb can cause cough).
Assessment Procedure
•Inspection •Palpation •Percussion •Auscultation • •Review the thoracic landmarks
Inspection:
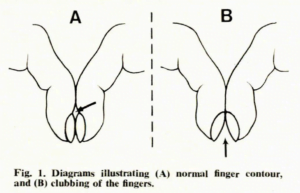
Skin ( central vs peripheral), chest ( barrel ), nail bed ( normal vs clubbed), intercostal spaces ( retraction or bulging), respiration rate, and respiration pattern. Note rhythm and chest movement)
Diaphragm vs thoracic muscle breather ( men and children tend to be diaphragmic as women tend to be thoracic)
Eupnea: normal RR
Tachypnea over 20 RR
Bradypnea lower 12 RR
Kussmal: regular ventilation to deep then tachy = acidosis
Cheyne Stoke: ventilation gradually increase then decrease follow apnea ( indication: CNS dysfunction r/t brain injury or CVA, CHF, coma, or dying)
Biot: irregular depth with apnea ( indication CNS dysfunction and brain injury)
A.P Ratio normal: 2 (chest) :1 ( side)

Fingernail:

Thoracic Landmark



Palpation
•Palpation •Percussion •Thoracic Expansion, and Tactile Fremitus
- Used finger pad or palm to assess skin temp, pain, mass, crepitus.
- thoracic expansion – place hand at 10th w/ thumb point toward spine at the intercosteral space. pt inhale deeply- thumb should move symmetrically apart at least 3-5cm. unlaterally lung expansion indicate air or fluid flilled or COPD

Tactile Fremitus
place palm with finger elevated in equal position on right and left lung field, instruct pt to say 99 down posterior chest wall bilaterally and asses strength if vibration.

Route

increase fremitus indicated fluid or solid structure in the lung: pneumonia, pleural effusion, or tumor.
Decrease fremitus indicated extra air trapped in the lung or pleural space; emphysema or pneumothorax
Percussion
purpose: determine lung tissue fill w/ fluid, solid, or air. Also, use to determine the position of the diaphragm or underlying organ.


Sound indication:
| •Resonant sound- Air-filled as in a normal lung sound •Flat sound– Over bone (sternum), over lung fields may indicate a massive pleural effusion •Tympany sound- Over the stomach and intestines (gas bubbles) •Dullness- Over kidney and liver normal, can be percussed over an atelectatic lung or consolidated lung •Hyper-resonant sound- Air trapping in the pleural space- emphysema, occasionally over a pneumothorax |

Auscultation
| Trachea- loud and harsh Bronchovesicular- medium intensity and pitch. equal in expiration and inspiration. b/w 1st and 2nd intercostal space. The vesicular- soft intensity and low pitch. longer and louder in inspiration |



Pleural effusion – excess fluid in the pleural space.
Pneumothorax – a buildup of air or gas in the pleural space.
Hemothorax – a buildup of blood in the pleural space.
| Not part of the assessment: but remember that snoring for children should be checked w/ PCP. Possible cause: OSA or Asthma and others which will complication development. |